Prostate cancer (PCa) is the second leading cancer diagnosis for men worldwide.1
In the U.S., it is the leading cancer diagnosis in men and the second leading cause of death.2 While PCa’s overall U.S. five-year survival rate is excellent at 98%, the disease at more advanced stages has a 30% five-year survival rate.2
The Prostate Testing for Cancer and Treatment (ProtecT) feasibility study, a randomized controlled trial, found that 95% of men with low and intermediate risk localized prostate cancer do not die of it within 10 years, irrespective of treatment.3 Because PCa can be slow-growing and indolent, differentiating those cases from the more aggressive prostate cancers that are more likely to lead to mortality is important.
The limitations of the PSA test’s sensitivity and specificity as well as indiscriminate use of the test in those who may not benefit from detection, static cutoff values guiding biopsy recommendations, and poor decision- making regarding treatment of low-grade disease, has led to PCa’s overdiagnosis and overtreatment, especially in the U.S.4
Within the past decade, multiparametric magnetic resonance imaging (mpMRI) has gained traction as a valuable adjunct in PCa risk stratification. While there are many current and potential future indications for its use (staging, therapy selection, local recurrence detection, and active surveillance), this article focuses on its value in the pathway to PCa diagnosis.
Limitations of Traditional Tools for PCa Detection
Total PSA has long been the primary screening test for PCa. It is used in conjunction with a digital rectal exam (DRE) to help determine which patients who may be at risk for prostate cancer to biopsy. Given the operating (sensitivity and specificity) characteristics of the test and the confounding diagnoses that can lead to PSA elevation, the positive predictive value (PPV) of PSA for PCa ranges from 25% to 40%.5 Secondary tests, including PSA kinetics and derivatives such as PSA velocity and PSA density, biomarkers such as urinary PCA3, and clinical algorithms, have been developed to improve PSA sensitivity and specificity.
Transrectal ultrasound guided biopsy (TRUS) is currently the standard procedure used for prostate biopsy. A drawback of it, however, is that it is blind, meaning that the ultrasound lacks the capability to distinguish abnormal from normal tissue in order to know exactly where and what to biopsy. A systematic approach is therefore used to obtain three cores from each of the four zones of the prostate. Even so, sampling error can lead to nondetection of 20% to 50% of clinically significant prostate cancer (csPCa) in a first biopsy.6 Although there is some variation in the literature in defining a csPCa, most studies agree it is a lesion predicted to be Grade Group (GG) of 2 or higher (equivalent to a Gleason score of 3+4=7). Serial TRUS biopsies also do not have an increased cancer detection rate.4
Table 1
Equivalent Grade Groups and Gleason Scores
| Group Grade | Gleason Score |
|---|
1 | 6 |
2 | 7 (3+4) |
3 | 7 (4+3) |
4 | 8 |
5 | 9-10 |
At the same time, estimates suggest that approximately 30% of PCa cases when first identified are slow-growing and indolent. Hence, there is the possibility of offering active surveillance rather than treatment for a low-risk subset of patients.7
There is also a need to more effectively identify patients who might benefit from a biopsy to detect significant prostate cancers while reducing unnecessary detection and biopsies of indolent cancers.6
mpMRI: What It Is
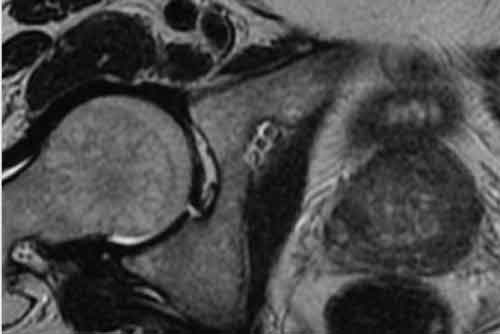
mpMRI combines anatomical sequences of T1- and T2-weighted MRI images with functional sequences (diffusion-weighted and dynamic contrast-enhanced images) in order to obtain three-dimensional images of the prostate.5, 6 The findings are then classified using the Prostate Imaging-Reporting and Data System (PI-RADS), which is currently in version 2.1 (the original was first released in 2011, and it has had two revisions since then). A higher PI-RADS score
indicates higher suspicion of clinically significant malignancy (Table 2). Lesions at higher risk for prostate cancer are then biopsied, using a variety of techniques.
Table 2
Prostate Imaging-Reporting and Data System (PI-RADS) – Classifications
PI-RADS | Likelihood of Cancer |
|---|
PI-RADS 1 | Very Low: clinically significant cancer is highly unlikely |
PI-RADS 2 | Low: clinically significant cancer is unlikely |
PI-RADS 3 | Intermediate: clinically significant cancer is equivocal |
PI-RADS 4 | High: clinically significant cancer is likely |
PI-RADS 5 | Very High: clinically significant cancer is highly likely |
mpMRI in the Clinical Diagnostic Pathway
Many studies have shown that mpMRI- and MRI-guided biopsies detect clinically significant prostate cancer (csPCa) and have decreased detection rates for clinically insignificant cases. There is, however, wide heterogeneity in these studies.4, 8 A 2019 metanalysis, for example, noted that average PPVs for GG ≥2 lesions are 12%, 48%, and 72%, which correlate to PI-RADS scores of 3, 4, and 5, respectively. Another meta-review of 43 studies noted pooled sensitivity and specificity for mpMRI of 91% and 37%, respectively, for GG ≥2 lesions.6, 8
mpMRI- and MRI-guided biopsies detect clinically significant prostate cancer (csPCa) and have decreased detection rates for clinically insignificant cases.
The European Association of Urology (EAU) was an early adopter of mpMRI technology for prostate cancer investigation. Currently, practice guidelines from the EAU and the American Urological Association include use of mpMRI as an adjunct in risk stratification for biopsy-naïve patients (pre-biopsy) as well as for those with rising PSA levels or other markers of persistent clinical suspicion following an initial negative TRUS biopsy.4, 8
The ability to forego biopsy for those with low risk scores (PI-RADS ≤2) varies by urologic society guidelines, patient characteristics, and ultimately comes down to a decision shared by doctor and patient.
Prebiopsy/Biopsy-Naïve Settings
The three landmark studies commonly cited in favor of the use of mpMRI in prebiopsy/biopsy-naïve patients are: PROMIS (PRostate Magnetic resonance Imaging Study); PRECISION (PRostate Evaluation for Clinically Important disease, Sampling using Image-guidance Or Not?); and the MRI-FIRST trials.
PROMIS, a prospective multicenter paired-validation cohort study, assessed the efficacy of mpMRI versus that of TRUS-guided systematic 12-core biopsy and the study’s reference standard of the template prostate-mapping (TPM) biopsy, in detecting clinically significant prostate cancers and reducing unnecessary biopsies. Study subjects were biopsy-naïve patients in whom there was viable clinical suspicion of PCa (due to elevated PSA levels, abnormal DRE, or a family history of PCa). Of the 576 men who underwent all three tests, 71% had prostate cancers detected by TPM, but only 40% were deemed clinically significant PCa (defined as a Gleason score of ≥4 + 3 [Grade Group 3] or a cancer core length of at least 6 mm). mpMRI tests were found to have a sensitivity of 93% versus 48% for TRUS. Using a broader definition of clinically significant as GG ≥2 or a cancer core length of at least 4 mm, the negative predictive value (NPV) for low-suspicion mpMRI was 74%. The authors concluded that using mpMRI to stratify risk prior to biopsy may reduce unnecessary biopsies by 27%, and that 18% more clinically significant cases of PCa may be detected compared to the TRUS biopsy.9, 10
PRECISION was a noninferiority trial that randomized 500 biopsy- naïve men to either a TRUS systematic (i.e., blind) or a targeted (mpMRI followed by MRI-guided) biopsy in those with clinical suspicion of PCa. The trial sought to determine which method might be more effective for detecting clinically significant (defined as GG ≥2) prostate cancer. Clinically significant PCa was detected in 38% of men in the targeted biopsy cohort compared to 26% of the systematic biopsy cohort, and 13% less clinically insignificant (GG=1) cancer was detected in the targeted cohort. However, 28% (n=71) of the men whose cancers were classified as PI-RADS 1 and 2 were not biopsied, calling into question the mpMRI’s NPV of 88.1%, and both targeted and systematic biopsies were not performed in the mpMRI-targeted cohort.9
MRI-FIRST was a prospective multicenter trial designed to investigate whether undergoing an mpMRI before a biopsy might improve csPCa detection in biopsy-naïve patients. The trial determined there was no significant difference in csPCa detection for systematic vs. targeted biopsy, but detection was higher when techniques were combined.4, 11
A 2020 systematic review by Sathianathen et al. investigating the NPV of mpMRI for csPCa (GG ≥2) in prebiopsy/biopsy-naïve patients noted a NPV of 91%. Still, in approximately 7% to 10% of cases, an mpMRI will fail to detect a csPCa without a subsequent biopsy due to reading failure, invisibility of lesions on mpMRI, or because the lesion was missed in the targeted biopsy.8, 12 Because of this, additional clinical indicators such as family history, pretest probability of PCa, and risk calculator scores are combined with lower PI-RADS scores to further stratify the risk. For example, adding a low PSAD (prostate specific antigen density) level (≤0.15 ng/ml/cc) can improve the NPV of the mpMRI.8
Repeat Biopsy Setting
mpMRI is recommended for individuals with persistent clinical suspicion (such as rising PSA levels) after a negative TRUS biopsy, if available, to decrease sampling error. For suspicious lesions on an mpMRI (PI-RADS ≥3), for example, a targeted biopsy is recommended that would sample the detected lesions, and there would be questionable value for an added systematic biopsy.4, 8 In this setting, subsequent mpMRI and targeted biopsy has detected csPCa in approximately 10% to 40% of those who initially had a negative TRUS.4 Like the biopsy-naïve group with low PI-RADS scores, concurrent indicators can be used to risk-stratify the need for biopsy. Importantly, if biopsy is deferred due to mpMRI findings, continued clinical and laboratory follow-up is indicated.
Limitations and Future Directions
Clinically, efficacy of mpMRI is balanced with its limitations, which include expense, availability, and potential renal impairment and inconvenience of intravenous line placement when contrast is used. Additionally, standardization of radiologist training to ensure consistent interpretation of mpMRI is of paramount importance, as inter-reader reliability can vary.
Currently, biparametric MRI, which uses only two modalities and does not use contrast, is being studied for use in PCa detection. Preliminary studies of biparametric MRI show comparable sensitivity and specificity with multiparametric MRI, but it is unclear if there will be a significant difference in the research setting compared to clinical practice setting.4, 13
The wide ranges of PPV and NPV in mpMRI results noted in the literature vary depending on patient populations, prevalence, indication for use, accessory tests, and inherent limitations of study design. For example, prebiopsy mpMRI is not indicated for very low-risk patients (based on clinical, biochemical, and family history information) as the sensitivity would result in a greater number of false positives. As with all tests, the external validity of the study population, or the ability to generalize the conclusions of a study to other populations that were not studied, is important when applying to clinical practice, and thus needs to be considered in insurance medicine and underwriting.
Underwriter Considerations
Given the evolution of indications for the use of mpMRI in PCa diagnosis, underwriters should have some familiarity with this modality. There are several considerations, however, as more cases will be detected with mpMRI at different stages of the path to a diagnosis.
There is no consensus that PI-RADS scores of 1 or 2 for biopsy-naïve patients means they can forgo biopsy.
mpMRI is just one tool to consider in those with abnormal PSA trends. Look at the overall picture for risk assessment: age, family history of prostate cancer, and data points such as results of a DRE, PSA kinetics, PSA density, prostate health index, risk calculators, and genetic biomarkers (if allowed).
Standards of care vary from country to country, and indications for use of mpMRI will differ depending upon the geography.