Incidence of thyroid cancer has been increasing worldwide, largely due to greater use of body imaging with ultrasound and subsequent fine needle aspiration (FNA) for incidentally discovered thyroid nodules.1
Papillary thyroid cancer (PTC), a type of differentiated thyroid cancer (DTC), is solely responsible for the increase in cases,2 accounting for nearly 90% of all thyroid cancers.2, 3 Another important factor has been the increased diagnosis of a PTC variant – follicular variant papillary thyroid cancer (FVPTC). However, it was recently recognized that a percentage of these cases were tumors with very low potential for malignancy, and so were reclassified from a cancer to a neoplasm. This article explores some of the newer nomenclature for differentiated thyroid cancers and current issues in assessing critical illness claims for them.
Introduction
Thyroid cancer can arise from thyroid follicular or parafollicular C cells. Differentiated thyroid cancer (DTC) arises from the follicular cells and includes papillary thyroid cancer (PTC), follicular thyroid cancer (FTC), and variants of both. These cancers generally have excellent prognoses, with 10-year survival rates in excess of 90% to 95%.3 Poorly differentiated thyroid cancers, which probably arise from either PTC or FTC, have worse outcomes, with 10-year survival rates of around 50%. Anaplastic thyroid cancer, one such cancer, is a rare but aggressive undifferentiated tumor arising from thyroid follicular cells with less than 10% survival at five years.4
Differentiated Thyroid Cancers
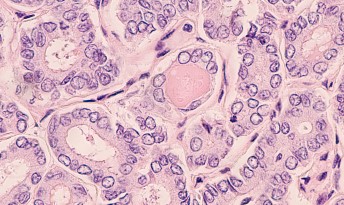
The histology of PTC is characterized by a papillary growth pattern. Papillae are tongue-shaped structures with one or two layers of tumor cells surrounding a well-defined fibromuscular core. Follicles are usually absent. The nuclei of the malignant cells appear large, oval, crowded, and overlapping, and may contain hypodense powdery chromatin, pseudoinclusions, or nuclear grooves (also called “orphan Annie eyes”). PTC is typically unencapsulated.
PTC is also often multifocal, either due to lymphatic spread within the thyroid gland or field change, with the development of synchronous tumors which are locally invasive and can spread to local lymph nodes in the neck. Distant spread may also be present in up to 10% of cases at the time of diagnosis, with lung and bone being common sites.
A scoring system based on tumor size and shape, membrane irregularities, and characteristics of the chromatin is used to make the diagnosis of PTC.
FTC has a completely different histological appearance from PTC. The architecture in good prognosis tumors shows well-differentiated epithelium forming follicles containing colloid. In poor prognosis tumors, the cells are poorly differentiated, growing as a solid mass without forming follicles. The nuclei do not have the features seen in PTC. There can be invasion of the blood vessels and also the tumor capsule.
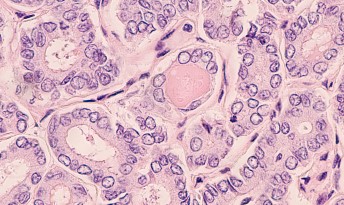
Histopathology of Follicular Thyroid Cancer – good prognosis subtype showing follicular architecture
Diagnosis of Differentiated Thyroid Cancer
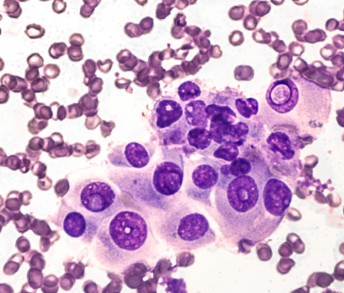
When thyroid cancer is suspected, an ultrasound exam is performed, followed by fine needle aspiration of the thyroid lump. Microscopic examination of the cells enables the pathologist to recognize the typical changes of the nuclei associated with PTC.
For follicular tumors, however, it is not possible for a pathologist to tell the difference prior to surgery between a benign follicular adenoma and malignant FTC. Examination of the thyroid lobe after surgery to identify the tumor capsule and assess vascular invasion is required for a diagnosis of FTC.
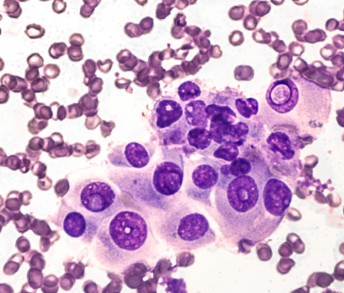
Fine Needle Aspiration from papillary thyroid cancer with the cancer cells showing the typical appearance of Orphan Annie eyes
Staging and prognosis
There are several systems for staging DTC. Each uses a core set of data that usually includes age at diagnosis, size of the primary tumor, extent of local extrathyroidal extension, and the presence or absence of distant metastases. However, there are sufficient differences among the systems that they are not interchangeable. The TNM system shown in Table 1 appears to be the best for predicting disease-specific mortality.5
Outcomes, stage for stage, are very similar for PTC and FTC. Mortality from PTC increases progressively with advancing age, starting around age 35. Using the cut-off of age 55 appears to be the most reliable for categorizing risk.6 Thyroid cancers arising from the follicular cells of the thyroid gland, however, display a spectrum of biological behaviors ranging from papillary microcarcinoma in the elderly, for which prognosis is generally excellent, to the highly lethal anaplastic thyroid cancer, which has a 10% to 20% survival rate at one year.
The subtypes of PTC and FTC have important influences on outcomes. Excellent outcomes are associated, for example, with non-invasive encapsulated FTC and with follicular variant papillary thyroid cancer (FVPTC). The more aggressive variants – poorly differentiated thyroid cancer, tall cell variant, hobnail variant, and columnar cell variant – tend to have poorer outcomes. Several other histological features, such as perineural invasion, multifocal disease, and high mitotic rate, may influence the prognosis as well. However, these histological features are not included in the staging system of the American Joint Committee on Cancer (AJCC) as there are no absolute pertinent cut-points.
Tables 1 and 2 illustrate the AJCC staging system,7 which is based on TNM (tumor, node, metastasis) parameters (Table 1) and uses the age 55 cutoff for the prognostic subgroups (Table 2). Pathological staging of cancers is based on findings at surgery for extrathyroidal spread and the pathology of the surgical specimen. Nodal involvement and distant metastatic spread may only be detected by radioactive iodine scans which are performed one to three months after surgery.
In addition to staging at diagnosis, the American Thyroid Association8 also recommends additional staging to predict risk of recurrence, risk of persistent disease, and to modify the risk estimate based on response to therapy. Factors such as serum thyroglobulin four to six weeks after initial surgery, calculated thyroglobulin doubling time, radioactive iodine uptake, and avidity of FDG uptake on PET scans may also influence the prognosis.
Table 1
AJCC TNM Staging for PTC, FTC, Poorly Differentiated, Hurthle, and Anaplastic Thyroid Cancers
Category | Criteria |
|---|
T1 | Tumor 2 cm or less limited to the thyroid gland |
T2 | Tumor >2 cm and up to 4 cm limited to the thyroid gland |
T3 | Tumor >4 cm limited to the thyroid gland or gross extrathyroidal extension invading only infrahyoid (strap) muscles |
T4 | Includes gross extrathyroidal extension |
N0 | No evidence of locoregional lymph node metastasis |
N1 | Metastasis to regional nodes |
M0 | No distant metastasis |
M1 | Distant metastasis |
Source: AJCC Cancer Staging Manual 8th Edition
Table 2
AJCC Prognostic Stage Groups for Differentiated Thyroid Cancer (PTC and FTC) Incorporating Age With TNM Staging
When age at diagnosis is… | And T is… | And N is… | And M is… | Then the stage group is… |
|---|
<55 years | Any T | Any N | M0 | I |
<55 years | Any T | Any N | M1 | II |
55+ years | T1 | N0/ NX | M0 | I |
55+ years | T1 | N1 | M0 | II |
55+ years | T2 | N0/ NX | M0 | I |
55+ years | T2 | N1 | M0 | II |
55+ years | T3 | Any N | M0 | II |
55+ years | T4a | Any N | M0 | III |
55+ years | T4b | Any N | M0 | IVA |
55+ years | Any T | Any N | M1 | IVB |
Source: AJCC Cancer Staging Manual 8th Edition
Most patients with DTC do not die of it: long-term cancer- related mortality is less than 5%.3 Multiple studies confirm that DTC mortality increases progressively with advancing age but even older patients (65+ years) in the SEER database still demonstrate 95% survival at five years.
Tumor size is important for prognosis. Tumors of less than 1.5 cm in size are universally cured, but mortality increases with tumor size. Twenty-year mortality for tumors measuring between 2.0 cm and 3.9 cm, for example, is 6%, and increases to 50% for tumors 7.0 cm or larger.9 Involvement of the regional lymph nodes is also an important adverse factor, particularly when associated with T4 tumors or M1 disease. However, small volume nodes have little impact on survival particularly at younger ages (<45 years), as they can be effectively eradicated by radioactive iodine therapy.
Follicular Variant PTC (FVPTC)
There are more than 10 variants of PTC,10 including follicular (the most common), tall cell (more aggressive), insular, hobnail, and diffuse sclerosing variants (Table 3). FVPTC, which represents 30% to 40% of all cases,11 has an architecture of follicles rather than papillae, and the malignant follicular cells show the characteristic features of PTC.
There are two main subtypes of FVPTC: encapsulated (EFVPTC), which represents the majority of FVPTC, and non-encapsulated or infiltrative (NFVPTC). The two subtypes have clearly different clinical and biological behaviors. They also differ in their molecular profiles, with the BRAF V600E mutation seen in the infiltrative tumors and the RAS mutation in the encapsulated tumors.
Two-thirds of infiltrative FVPTC cases exhibit lymph node spread, whereas EFVPTC rarely (5%) involves lymph nodes. EFVPTC may also show signs of invasion of the tumor capsule, of blood vessels within the capsule, or of the adjacent thyroid tissue. Minimal invasion of the capsule slightly increases the risk of recurrence, but invasion of the lymphatics and/or blood vessels – particularly if extensive (>4 foci) – greatly increases the risk of recurrence, spread, and mortality.
A substantial number of FVPTCs are neither encapsulated nor infiltrative, but instead are partially encapsulated or well-demarcated. They have a similar molecular profile to EFVPTC, with the RAS mutation seen in nearly half the cases (46%) and no BRAF V600E mutation seen.
Table 3
PTC Variants12
Variant; | Molecular Alteration | Clinical Behavior |
|---|
Papillary microcarcinoma <1 cm | BRAF V600E | Excellent |
Encapsulated | Not specified | Excellent |
Follicular | RAS mutation | Excellent |
Diffuse sclerosing | RET/PTC | Less favorable |
Tall cell | BRAF V600E | High risk |
Columnar cell | Not specified | High risk |
Cribriform-morular | APC | Excellent |
Hobnail | BRAF V600E | High risk |
Fibromatosis/Fasciitis-like stroma | Not specified | No information |
Solid/Trabecular | RET/PTC3 | High risk |
Oncocytic | Not specified | Less favorable |
Spindle cell | Not specified | No information |
Clear cell | Not specified | No information |
Warthin-like | Not specified | No information |
Source: WHO Classification for Thyroid Tumors, fourth edition.
Non-Invasive Follicular Thyroid Neoplasm with Papillary Nuclear Features (NIFTP)
In the last 20 to 30 years, incidence of encapsulated thyroid tumors has risen two to threefold and now represents 10% to 20% of all thyroid cancers in Europe and North America. These tumors generally have an indolent course and following limited surgery (removal of the affected lobe rather than the whole thyroid gland), they very rarely relapse or spread to distant sites. To avoid overdiagnosis and overtreatment, these tumors were downgraded from cancer to neoplasm in 2017.
In 2016, an international working group of expert thyroid pathologists convened by the National Cancer Institute reported on a study of 109 patients diagnosed with EFVPTC.13 At a median follow-up of 13 years there were no episodes of recurrences or spread in these patients. This was not, however, the case for patients with the invasive form of FVPTC. Because of these results, the working group recommended that EFVPTC be called “non-invasive follicular thyroid neoplasm with papillary- like nuclear features” (NIFTP).
This change in nomenclature and classification was subsequently accepted by the World Health Organization (WHO) and was included in the 4th edition of the WHO Classification of Tumors of Endocrine Organs, published in 2017.14 NIFTPs are now usually treated by removal of one lobe of the thyroid and radioactive iodine treatment is omitted.
Diagnosis of NIFTP is based on strictly defined inclusion and exclusion criteria, which are outlined in Table 4. The assessment of whether a tumor is non-invasive or invasive cannot be made until the tumor and its surrounding capsule have been removed by lobectomy. The pathologist needs to examine the entire capsule carefully to determine if there is any invasion by cancer cells or any lymphovascular invasion.Thus, the diagnosis can only be made after surgery, not pre-operatively.
The average size of an NIFTP is 3 cm, but they can vary from microtumors (<1 cm) to as large as 10 cm. They can also be multifocal or affect both lobes, and can be found in a thyroid gland containing an invasive tumor.
From the perspective of assessing critical illness (CI) claims, it is important to be aware that not all EFVPTC cases have been downgraded from cancer to NIFTP. The strict criteria for diagnosing NIFTP highlight that there should be no invasion into the capsule or into the adjacent thyroid gland for well-circumscribed tumors.
Table 4
NIFTP Inclusion and Exclusion Criteria13
Inclusion Criteria |
The tumor must be well-demarcated, with discrete interface with the surrounding thyroid tissue. There can be three scenarios: |
|
|
|
Appearance of the nuclei as seen in PTC. The features can be subtle and are often easier to assess in areas of small follicles or near the tumor periphery. |
Exclusion Criteria |
Invasion with complete tumor capsule penetration. For well-circumscribed tumors lacking a fibrous capsule, infiltration of tumor cells into adjacent uninvolved thyroid tissue. Also, lymphatic and/or vascular invasion defined by tumor cells within an endothelial lined space in the tumor capsule or in vessels outside the tumor. |
Pattern of growth not showing follicular architecture although up to 30% solid, trabecular, or insular appearance is allowed. |
Papillary structures. |
High-grade features with psammoma bodies (dead calcified papillae), tumor necrosis, or high mitotic index (i.e., three or more mitoses per 10 high-power fields). |
Source: Nikorov et al. Nomenclature Revision for Encapsulated Follicular Variant of Papillary Thyroid Carcinoma: A Paradigm Shift to Reduce Overtreatment of Indolent Tumors.
Assessing EFVPTC Claims
Case 1: EFVPTC that does not meet NIFTP criteria
History: A 25-year-old man presented with a persistent non-tender 4-5 cm lump in the right lobe of the thyroid gland. There were no palpable lymph nodes in the neck. Following a multidisciplinary team (MDT) discussion of the ultrasound and fine needle aspirate cytology results, the right lobe of the patient’s thyroid gland was removed.
Pathology: Gross pathology revealed a well-defined lesion extending through the entire right lobe, measuring 45 x 35 x 26 mm. Microscopy determined that it was an encapsulated follicular lesion predominantly consisting of microfollicles, many containing colloid, and that there were a few rudimentary papillae. The capsule was relatively thin and in two blocks (sections) there was suspicion of possible capsular invasion. In several blocks there was also suspicion of vascular invasion.
Provisional diagnosis: EFVPTC confined to the thyroid gland with a clearance of 0.1 mm. There were no lymph nodes present. Stage: pT3a and R0 (clear margins).
The case was also sent to an expert thyroid pathologist who agreed that the tumor was a well-defined encapsulated mass. The pathologist noted that there were multiple foci of FVPTC but did not feel there was evidence of vascular invasion. However, there were some epithelial components extending into but not penetrating through the fibrous capsule.
Conclusion: Multifocal EFVPTC with tumor cells within the capsule but no vascular invasion. Stage: pT2 NX MX and R0.
The MDT recommended completion of the thyroidectomy followed by radioactive iodine treatment. Pathology examination of the left lobe did not show any cancer.
Key points for assessing the critical illness claim:
The tumor had a complete capsule (i.e., encapsulated). Note that presence of a capsule does not exclude invasive cancer.
The tumor was multifocal.
Expert opinion was that vascular invasion was absent.
There were tumor foci in the capsule (this excludes diagnosis of NIFTP).
Size cannot differentiate between NIFTP and invasive thyroid cancer as NIFTP can be 4 cm or larger in up to 5% of cases.
Treatment was provided as for invasive thyroid cancer.
This case was accepted as a valid critical illness claim as this cancer was showing signs of invasion with involvement of the tumor capsule.
Case 2: Partially encapsulated FVPTC
History: A 36-year-old woman with a past history of multinodular goiter and thyrotoxicosis presented with a persistent lump on the left side of her neck after a throat infection. An ultrasound scan showed an indeterminate heterogenous well-defined nodule in the left lobe of the thyroid, measuring 18 x 10 mm.
Fine needle aspirate cytology showed papillary clusters of cuboidal-to-columnar cells supported by fibrovascular stroma. The nuclei showed features suspicious for PTC. She underwent removal of the left lobe of her thyroid.
Pathology: Gross pathology revealed a 15 x 12 x 22 mm nodule close to the surface of the thyroid gland. Microscopy showed a partly encapsulated follicular variant of papillary thyroid cancer. The capsule was fibrous and in areas ill-defined. The cells showed overlapping nuclei with grooves and inclusions. Vascular invasion was suspected, as several foci of intracapsular cells were seen to mingle with vessels, but interpretation was complicated by the granulation tissue response to previous fine needle aspiration. Definite evidence of vascular invasion was absent. There was also no evidence of capsular invasion or extension beyond the thyroid gland. The tumor extended to within 0.22 mm of the thyroid capsule.
Conclusion: Partially encapsulated and clearly demarcated FVPTC with suspected vascular invasion but no capsular invasion. Stage: pT2 (22 mm) NX MX.
Based on suspicion of vascular invasion, the remaining right lobe of her thyroid was removed, followed up by radioactive iodine treatment. The pathology of the right lobe was negative for cancer.
Key points for assessing the critical illness claim:
- The capsule was incomplete and ill-defined in areas, therefore partially encapsulated.
- The tumor was demarcated and there was no sign of diffuse infiltration.
- There was no invasion of the capsule.
- There was suspicion of vascular invasion as several foci of intracapsular cells were seen to mingle with vessels. The interpretation was compromised by the after-effects of fine-needle aspiration with granulation (healing/scar) tissue.
- Treatment was provided as for higher risk tumor, with completion of the thyroidectomy and radioactive iodine therapy.
This case was accepted as a valid critical illness claim, as it was reasonable to conclude there was vascular invasion within the tumor capsule.
Case 3: Non-encapsulated FVPTC
The current approach for assessing critical illness claims for EFVPTC without evidence of tumor capsule invasion is to view it as a non-cancer.
In another brief case example, gross pathology of a thyroid tumor showed a nodule measuring 14 x 7 x 5 mm. Microscopy revealed features typical of NIFTP, with cells showing nuclear elongation, overlapping, grooves, and occasional intracytoplasmic nuclear pseudoinclusion. The tumor was well-circumscribed and demarcated but non-encapsulated. No vascular invasion or extrathyroidal extension was seen.
Upon review of the claim, the terminology in the pathology report was felt to be consistent with what is acceptable for the diagnostic criteria of a NIFTP. This claim was therefore determined not to meet the definition of cancer as defined by the policy provision, as there was no evidence of invasion nor was the neoplasm diffuse in nature.
Case 4: Tumors with uncertain malignant potential
History: A 41-year old woman presented with a 4 cm lump in the left side of her thyroid. She had previously undergone a right hemithyroidectomy 24 years earlier for a benign lesion. Ultrasound was indeterminate and fine needle aspirate cytology could not distinguish between follicular neoplasm and a benign lesion. The pathologist was also of the opinion that papillary thyroid cancer could not be excluded. She underwent removal of the remaining left lobe of her thyroid.
Pathology: Gross pathology showed a well-circumscribed nodular lesion measuring 27 x 33 mm. Microscopy confirmed a circumscribed and encapsulated nodule with closely packed follicles and a predominantly microfollicular growth pattern. There was a well-formed thick fibrous capsule, and no cytological features to suggest papillary carcinoma. There were also three separate small nodules just outside the capsule with similar appearance to the main tumor nodule, suspicious for extracapsular spread although extensive examination of the capsule did not show any growth within the capsule. It was noted that the background thyroid tissue had a vaguely nodular appearance with some nodules appearing similar morphologically to the main nodule although at some distance from it. The extracapsular nodules could represent compressed background nodular hyperplasia.
The tumor was limited to the thyroid gland and was clear of the surgical margin by 0.1 mm. No lymphovascular invasion was seen and all three lymph nodes were clear.
The report noted that at worst, the appearance could be consistent with minimally invasive follicular carcinoma, provisional stage pT2 N0. The case was sent to an expert thyroid pathologist.
Conclusion: Following discussion among members of the MDT, the surgeon wrote that this tumor was best described as “tumor of unknown malignant potential,” but that some features would fit with the diagnosis of minimally invasive thyroid carcinoma. This was therefore accepted as the final working diagnosis.
Key points for assessing the critical illness claim:
The tumor was an encapsulated lesion with three separate nodules of similar appearance outside the tumor capsule within the adjacent thyroid gland.
Although the capsule was intact, it was deemed reasonable to assume that these nodules represented invasive spread within the thyroid gland. Although the pathologist could not see invasion of the capsule, it was impossible to assess the whole capsule in detail, so it was possible to miss an area of invasion.
The final claim decision was in alignment with the MDT’s decision that this was a minimally invasive cancer.
This case highlights the difficulty of making a clear diagnosis even for an expert thyroid pathologist. The key clinicians in this MDT (surgeon, pathologist, radiologist, and oncologist) took into consideration the clinical findings and pathology in order to reach a final diagnosis and decide upon a treatment plan. If there was doubt about the pathological diagnosis, they could have also asked for an opinion from a regional or national expert.
For follicular patterned thyroid tumors, such as this case, the WHO classification system recognizes there are tumors of “unknown malignant potential,” which describes the uncertainty of the biological behavior of these tumors. The recognized types are called:
Summary
For DTC CI claims, assessment of cancer invasion depends upon evaluation of the tumor capsule, vascular invasion, and local spread within the adjacent thyroid and the lymph nodes.
EFVPTC meeting strict inclusion and exclusion criteria, defined by an expert international panel of pathologists, are now known as NIFTP. Downgrading these tumors from cancer to neoplasm recognizes that many of the cases are non-invasive tumors with excellent prognoses and so can be safely managed by limited surgery. This will enable these patients to avoid the complications of removal of the whole thyroid gland and radioactive iodine therapy. From the insurance point of view, these neoplasms generally would not meet the strict definition of “cancer” as defined by most CI policy provisions. Nonetheless, these cases should be reviewed carefully to ensure accurate and fair adjudication.